By Mikaela Sullivan
July 2024
What is the Menopausal Transition?
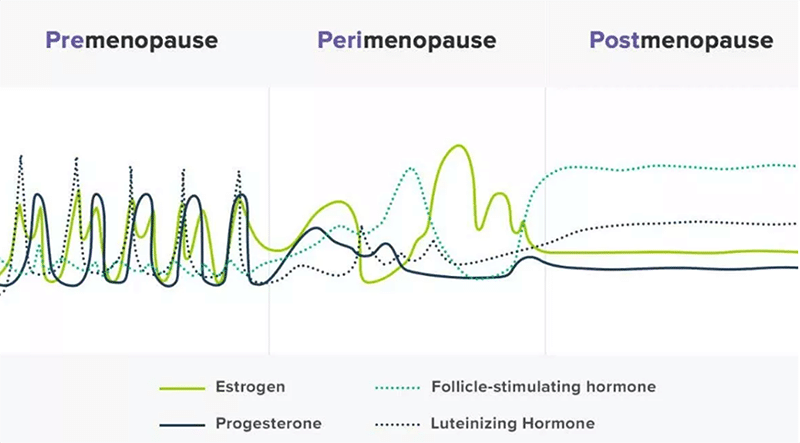
Many people are aware of menopause but may not fully understand the physiological changes that happen in the body and how they can affect health and well-being. Menopause marks the end of menstrual cycles, defined as the time from a woman's final period until 12 months later. Most women naturally reach menopause between the ages of 45 and 55. The period before menopause, known as perimenopause, is a time of fluctuating hormones, especially estrogen and progesterone, and can last anywhere from 5 to 10 years.
During this phase, menstrual cycles become unpredictable due to hormonal changes, including fluctuations in estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). This irregularity leads to various symptoms that can affect a woman's health in multiple ways.
Symptoms & Risk Factors
Due to these unpredictable hormonal shifts, women may experience a range of symptoms, from mild to more severe. Early-stage perimenopause is often characterised by peaks in estrogen, which can cause headaches, changes in body composition, and breast tenderness. As estrogen declines later in perimenopause and into menopause, women may experience fatigue, hot flashes, muscle weakness, sleep disturbances, cognitive changes, and joint stiffness.
Even during post-menopause, some women continue to experience symptoms related to low estrogen for 2-5 years. However, the risks associated with menopause go beyond symptoms.
Cardiovascular Disease Risk
The decline in estrogen during menopause has direct effects on the cardiovascular system. Blood vessels may become stiffer, and inflammation of the blood vessel walls can increase, leading to a higher risk of heart disease and stroke. Hormonal changes also contribute to weight gain, particularly around the organs, along with increased blood pressure, insulin resistance, and cholesterol levels.
Osteoporosis Risk
The reduced production of estrogen also affects bone health, decreasing bone formation and leading to a higher risk of osteoporosis. Many women experience a decrease in physical activity and muscle mass during this time, further contributing to the decline in bone density. Without the mechanical stimulus needed to build new bone cells, the risk of bone fractures increases significantly. It is estimated that some women may lose 3-5% of their bone mass annually in the 5-8 years following menopause.
The Role of Exercise in the Menopausal Transition
Regular exercise can be one of the most effective ways to combat the risks associated with menopause. Whether it's strengthening muscles, improving bone density, or maintaining cardiovascular health, exercise offers multiple benefits.
Strength Training
Resistance (strength) training is especially beneficial for menopausal and postmenopausal women. Studies show it improves:
- Muscular strength and mass
- Bone strength
- Functional capacity
- Quality of life
It can also reduce the frequency of hot flashes, decrease fat mass, and improve waist and hip measurements. However, the intensity and frequency of strength training matter for maintaining and improving bone and muscle mass. Working with a professional to develop an effective routine is key.
Impact Exercise
For women at risk of bone loss, impact exercises (such as jumping or stepping) combined with strength training can significantly improve bone density in the hip and spine. However, it's important to consult a health professional before beginning this type of exercise to ensure it's safe based on your individual risk factors for fractures, balance, and medical history.
Aerobic Exercise
Continuous aerobic exercise, like walking, swimming, or cycling, helps improve cardiorespiratory fitness, reduce total body fat, and improve waist-to-hip ratio. These changes help reduce the risk of cardiovascular disease, which becomes more prominent after menopause.
High-Intensity Interval Training (HIIT)
HIIT, which involves short bursts of intense activity followed by rest periods, has shown great promise for menopausal women. It can:
- Decrease blood pressure
- Improve cholesterol levels
- Regulate blood sugar
- Boost cardiovascular fitness
Research indicates that HIIT on a stationary bike may be more effective than running for improving overall health and well-being during menopause.
Sprint Interval Training (SIT)
Sprint Interval Training (SIT) typically involves short, high-intensity sprints of 8-12 seconds, followed by equal rest periods. This form of training has demonstrated significant benefits for women going through the menopausal transition, including:
- Reduced artery stiffness
- Decreased fat mass
- Lower resting heart rate
It also enhances muscle mass and aerobic fitness, providing a well-rounded approach to improving overall health.
Final Thoughts
As women go through the menopausal transition, exercise becomes a vital tool in managing the associated risks and symptoms. A balanced exercise program combining strength training, aerobic activity, and high-intensity intervals can help maintain bone density, improve cardiovascular health, and enhance overall quality of life.
If you're entering menopause, or are already in the menopausal transition, consult an Accredited Exercise Physiologist to develop an exercise plan tailored to your unique needs. Embrace this phase with strength, knowledge, and movement! You've got this!




